Complete Guide to Automation for Dental Practices: Boost Efficiency & Patient Care in 2026
by Design Delulu Editorial · September 26, 2025
Smart, fast, and measurable. Here's how Automation helps Dental Practices win.
In today's competitive dental landscape, practices that embrace intelligent automation aren't just saving time—they're fundamentally transforming patient experiences while dramatically reducing operational overhead. The difference between thriving and merely surviving often comes down to how effectively a practice can scale personalized care without proportionally scaling staff costs. Automation for dental practices has evolved far beyond simple appointment reminders; it now encompasses everything from patient communication workflows and insurance verification to treatment plan follow-ups and reputation management, creating a seamless ecosystem that allows dental professionals to focus on what they do best: providing exceptional clinical care.
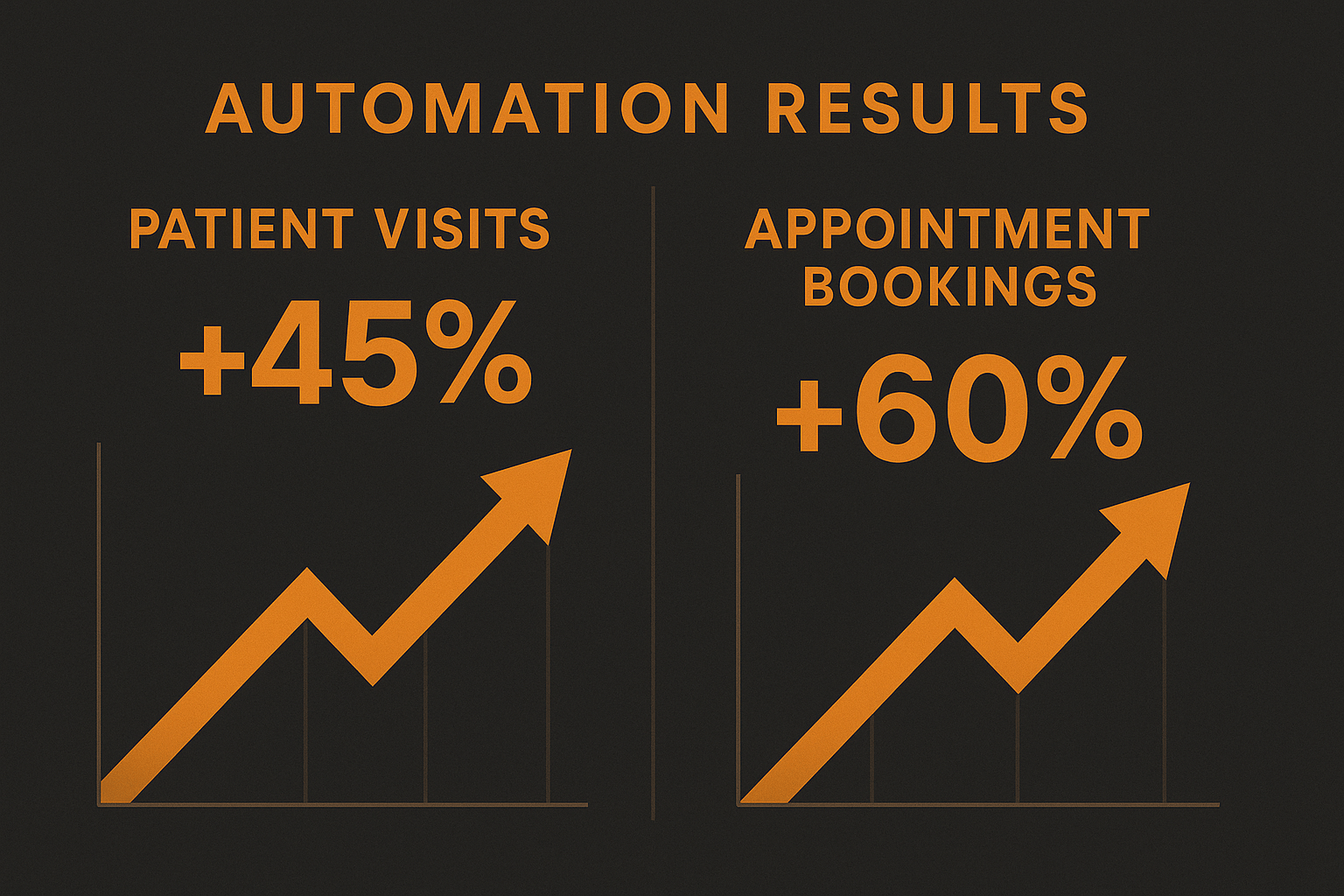
The strategic implementation of automation delivers measurable competitive advantages that compound over time. Practices implementing comprehensive automation systems report 40-60% reductions in administrative workload, 25-35% improvements in appointment show rates, and significant increases in case acceptance rates due to timely, personalized follow-up communications. More importantly, automation creates consistency in patient touchpoints that would be impossible to maintain manually, ensuring every patient receives the same high-quality experience regardless of front-desk staffing fluctuations. As patient expectations continue to rise and talented administrative staff becomes increasingly difficult to retain, automation isn't just a nice-to-have—it's becoming the foundation of sustainable, scalable dental practice growth.
Why Dental Practices Need Automation Now More Than Ever
The dental industry faces unprecedented challenges in 2026 that make automation not just beneficial but essential for survival. Staffing shortages continue to plague practices nationwide, with dental administrative positions remaining unfilled for an average of 90 days. Meanwhile, patient expectations have shifted dramatically—today's patients expect the same seamless digital experiences from their dental office that they receive from their favorite retailers and service providers. They want instant appointment confirmations, mobile-friendly payment options, and proactive communication about their oral health needs.
Traditional manual processes create bottlenecks that directly impact revenue and patient satisfaction. When front desk staff manually call to confirm appointments, send treatment plan reminders, or follow up on outstanding balances, these critical tasks often fall through the cracks during busy periods. A missed appointment costs the average dental practice between $200-$400 in lost revenue, and practices without automated recall systems lose approximately 30% of patients who need periodic cleanings simply because they forget to schedule. The financial impact compounds quickly—a single-dentist practice losing just five patients per week to preventable no-shows or lack of follow-up sacrifices roughly $50,000-$100,000 annually.
Beyond the direct financial implications, manual administrative work creates significant opportunity costs. Every hour your highly-trained team spends on repetitive tasks like insurance verification, appointment reminders, or data entry is an hour not spent on high-value activities like treatment planning consultations, patient education, or relationship building. Automation liberates your team to operate at the top of their license, focusing on interactions that require human judgment, empathy, and expertise. This shift not only improves job satisfaction and reduces burnout but also creates a more profitable practice model where staff time aligns with revenue-generating activities.
The data collection and analysis capabilities of modern automation systems provide another compelling advantage. Automated systems capture detailed information about patient behavior, communication preferences, and response patterns that would be impossible to track manually. This intelligence enables increasingly sophisticated patient engagement strategies—from identifying patients most likely to accept cosmetic treatment plans to optimizing appointment reminder timing based on individual response patterns. Practices leveraging automation analytics report 15-20% improvements in treatment acceptance rates and significant increases in preventive care adherence simply by delivering the right message at the right time through the right channel.
Core Automation Systems Every Dental Practice Should Implement
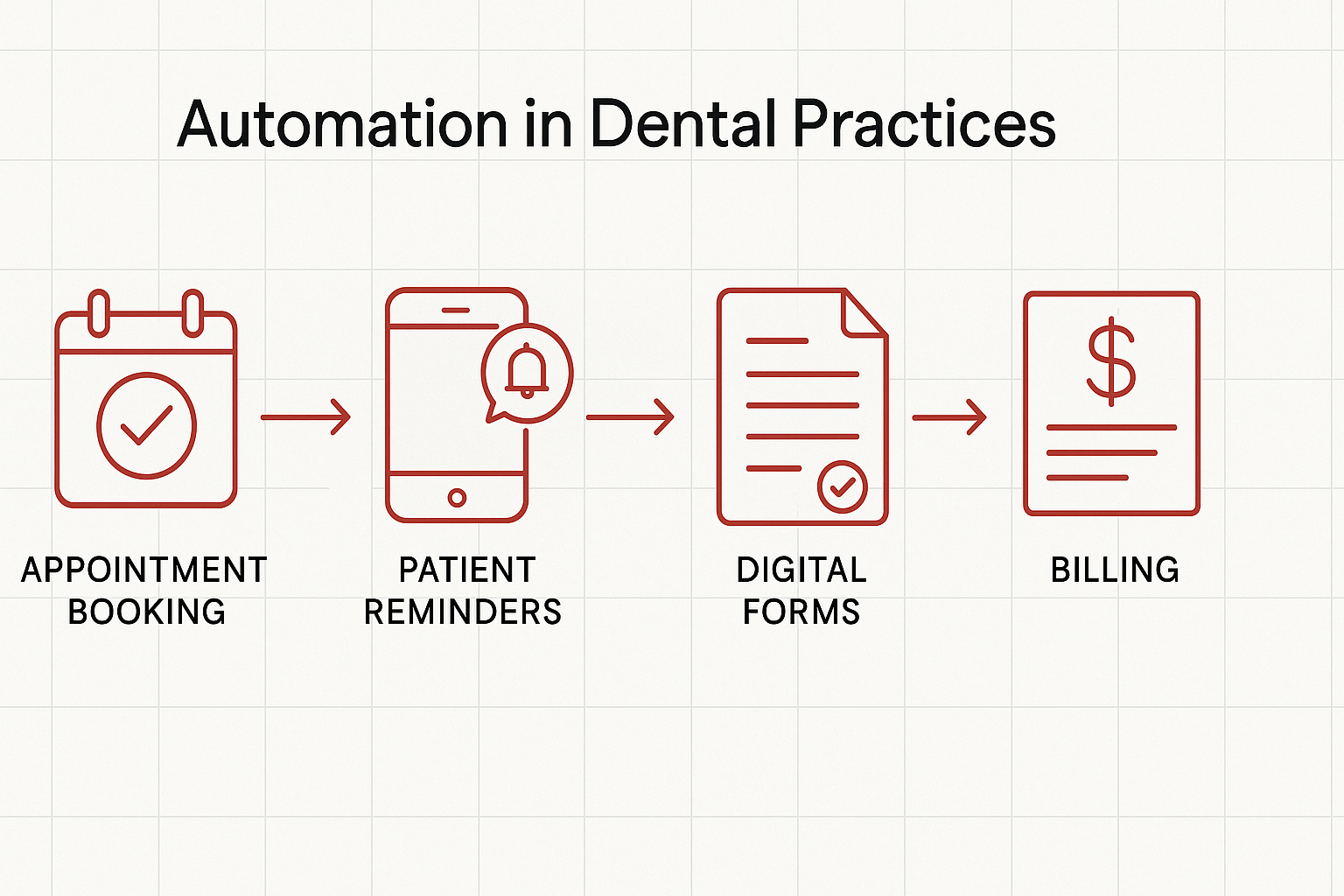
Building an effective automation infrastructure for dental practices requires a strategic, layered approach that addresses the most impactful operational areas first. The foundation begins with patient communication automation—the system that touches every patient at multiple points throughout their journey with your practice. This includes automated appointment confirmations and reminders delivered via SMS, email, and voice calls based on patient preference, post-visit follow-up messages checking on patient comfort and satisfaction, treatment plan reminders for accepted procedures not yet scheduled, and recall notifications for patients due for their next hygiene visit or periodic examination.
The second critical layer focuses on patient onboarding and intake workflows. New patient acquisition costs continue to rise, making it essential to convert inquiries efficiently and create positive first impressions. Automated onboarding sequences should trigger immediately when a new patient schedules, sending welcome messages with practice information, digital forms for medical history and consent documents, insurance verification requests, and pre-visit instructions or educational content relevant to their appointment type. By automating these touchpoints, practices reduce no-show rates for first appointments by up to 45% while simultaneously reducing the administrative burden of phone-based intake processes.
Revenue cycle automation represents the third essential pillar, addressing one of the most time-consuming and uncomfortable aspects of dental practice management. Automated systems can handle insurance eligibility verification before appointments, estimate patient portions based on benefits and fee schedules, send payment reminders for outstanding balances with convenient online payment links, and automatically segment patients by balance age for appropriate collection communications. Practices implementing comprehensive revenue cycle automation typically see 25-35% reductions in accounts receivable aging and 20-30% improvements in collection rates, all while reducing the staff time dedicated to billing and collections by approximately 50%.
Marketing and reputation management automation completes the foundational automation stack. In an industry where online reviews influence approximately 84% of patients when choosing a dental provider, systematically collecting positive reviews and addressing negative feedback becomes critical. Automated review request campaigns can identify satisfied patients based on specific criteria—such as completed treatment types or positive feedback indicators—and send personalized review requests at optimal timing. Simultaneously, internal feedback loops can intercept potentially negative reviews, giving practices opportunities to address concerns before they reach public platforms. Practices with automated reputation management systems generate 3-5x more reviews than competitors, creating powerful social proof that drives new patient acquisition.
Strategic Implementation Framework for Dental Practice Automation
Successful automation implementation follows a proven methodology that minimizes disruption while maximizing adoption and results. The process begins with a comprehensive discovery and goal-setting phase where practices clarify specific outcomes, constraints, and success metrics. Rather than pursuing automation for its own sake, effective implementations start with clear business objectives—whether reducing no-show rates by a specific percentage, decreasing front desk workload to enable staff reduction through attrition, or improving case acceptance rates for specific treatment types. This goal-oriented approach ensures technology investments directly address practice pain points and deliver measurable returns.
The blueprint phase translates business goals into detailed automation strategies, system architectures, and measurement frameworks. This includes mapping patient journeys and identifying optimal automation touchpoints, selecting and configuring appropriate technology platforms, designing message templates and communication sequences that reflect practice voice and values, establishing integration points between automation systems and existing practice management software, and defining key performance indicators and tracking mechanisms. Investing adequate time in planning prevents costly pivots mid-implementation and ensures all stakeholders share a common vision for the automated future state.
Implementation proceeds through careful build and launch phases that prioritize quality and team readiness over speed. The most successful rollouts follow a phased approach, beginning with a single automation workflow—typically appointment reminders since they deliver immediate, visible value—and progressively adding complexity as teams gain confidence and competence. Each phase includes rigorous testing with staff volunteers or patient segments before full deployment, comprehensive training for all team members who interact with automated systems, clear documentation and standard operating procedures for ongoing management, and established feedback mechanisms so teams can report issues and suggest improvements. This measured approach prevents the overwhelming disruption that causes many automation initiatives to fail or be abandoned.
The optimization phase represents where automation delivers compounding returns over time. Rather than treating implementation as a one-time project, high-performing practices establish continuous improvement processes that refine and expand automation capabilities. This includes regular analysis of automation performance metrics against established benchmarks, A/B testing of message content, timing, and delivery channels to optimize response rates, progressive automation of additional workflows as team capacity allows, and strategic integration of new capabilities as technology platforms evolve. Practices committed to ongoing optimization consistently outperform those that implement automation once and leave it static, extracting 40-50% more value from the same technology investments.
Measuring Success: Key Performance Indicators for Dental Practice Automation
Establishing robust measurement frameworks ensures automation investments deliver promised returns and guides optimization efforts. The most important metrics align directly with practice financial performance rather than vanity metrics that don't impact the bottom line. Appointment show rates represent a primary KPI, measuring the percentage of scheduled appointments that patients actually attend. Practices should track this metric overall and segmented by appointment type, patient status (new versus existing), and reminder delivery method to identify patterns and opportunities. Effective automation typically improves show rates by 15-25 percentage points, directly translating to increased production and reduced schedule gaps.
Patient reactivation rates measure how effectively automation re-engages patients who have lapsed from active care. Track the percentage of patients past due for recall who schedule and complete appointments within specific timeframes—30 days, 60 days, 90 days. Automated recall campaigns consistently outperform manual outreach by 200-300%, converting lapsed patients who represent the most cost-effective source of production growth since they already know and trust the practice. Calculate the production value of reactivated patients to quantify automation's direct revenue impact.
Treatment acceptance velocity tracks how quickly patients move from treatment plan presentation to scheduled procedures. Automated follow-up sequences that provide education, answer common questions, and remove scheduling friction significantly compress acceptance timelines. Monitor the average days between treatment plan creation and procedure scheduling, the percentage of treatment plans scheduled within 30 days, and the overall acceptance rate for different procedure categories. Practices implementing automated treatment plan nurturing sequences report 20-35% improvements in acceptance rates and 40-50% reductions in average acceptance timelines.
Administrative time savings quantify automation's efficiency impact, though this metric requires more manual tracking effort. Periodically measure time spent on specific tasks—appointment confirmations, insurance verifications, payment follow-ups, review requests—both before and after automation implementation. Document baseline time investments for these activities, then remeasure at 30, 60, and 90 days post-implementation. Most practices discover 40-60% reductions in time spent on automated tasks, freeing 10-20 hours weekly that can be redirected to patient care or enable staff optimization through attrition rather than layoffs.
Patient satisfaction scores provide qualitative validation that automation enhances rather than diminishes patient experience. Survey patients about their satisfaction with practice communication, appointment scheduling convenience, and overall experience both before and after implementing automation. Counter-intuitively, most practices see patient satisfaction scores improve with automation implementation, as consistent, timely communications create better experiences than inconsistent manual outreach. Track Net Promoter Score (NPS) and specific satisfaction dimensions related to automated touchpoints to ensure technology enhances rather than replaces the human connection patients value.
Advanced Automation Strategies for Competitive Advantage
Once foundational automation systems operate reliably, forward-thinking practices can implement advanced strategies that create sustainable competitive differentiation. Intelligent patient segmentation enables hyper-personalized automation sequences based on patient characteristics, behaviors, and preferences. Rather than sending identical messages to all patients, segment audiences by treatment history, lifetime value, engagement patterns, insurance coverage, demographic factors, and past response behavior. Then design automation sequences specifically optimized for each segment—high-value patients might receive more personal touchpoints including video messages from their provider, while cost-conscious patients receive content emphasizing insurance coverage and flexible payment options.
Predictive analytics integration represents the frontier of dental practice automation, using historical data to identify patterns and optimize future actions. Advanced systems can predict which patients face the highest no-show risk based on past behavior, weather, time of day, and other factors, then automatically adjust reminder frequency or delivery methods for high-risk appointments. Similarly, predictive models can identify patients most likely to accept specific treatment types based on past acceptance patterns, demographics, and engagement behaviors, enabling targeted education campaigns that dramatically improve conversion rates. While these capabilities require more sophisticated platforms and data infrastructure, early adopters report 25-40% improvements over standard automation approaches.
Multi-channel orchestration ensures messages reach patients through their preferred communication channels at optimal times. Rather than defaulting to email or SMS for all communications, sophisticated automation systems test and learn individual preferences, then automatically route future messages through channels that generate the highest engagement for each specific patient. Some patients respond best to text messages in the evening, others prefer email mid-morning, while some still value phone calls for important information. Systems that automatically optimize channel selection based on past behavior generate 40-60% higher engagement rates than one-size-fits-all approaches.
Integration with clinical systems creates powerful automation possibilities that extend beyond administrative functions into direct care support. When automation platforms integrate bidirectionally with electronic health records, practices can trigger educational content based on diagnosed conditions, automatically send oral health tips relevant to specific procedures, remind patients about prescription medication protocols, and provide post-operative care instructions customized to their specific treatment. This clinical integration positions automation as a direct enhancer of patient outcomes rather than purely an efficiency tool, strengthening the value proposition and potentially supporting reimbursement through care coordination codes.
Overcoming Common Implementation Challenges
Despite clear benefits, dental practices frequently encounter predictable challenges during automation implementation that can derail initiatives without proper preparation. Staff resistance represents the most common obstacle, often stemming from fear that automation threatens job security or concerns that technology will depersonalize patient relationships. Address these concerns proactively by clearly communicating that automation aims to eliminate tedious tasks while preserving and enhancing roles that require human judgment and relationship skills. Involve staff in planning and implementation decisions, solicit their input on message content and workflow design, and celebrate early wins that demonstrate how automation improves rather than replaces their work.
Technology integration complexity creates implementation friction when automation platforms don't seamlessly connect with existing practice management systems. Evaluate integration capabilities carefully during vendor selection, prioritizing platforms with native integrations or robust APIs for your specific practice management software. Budget adequate time and potentially consulting support for integration setup and testing, as smooth data flow between systems is non-negotiable for automation success. Poor integration leads to duplicate data entry, synchronization errors, and abandoned implementations when staff lose confidence in system reliability.
Message fatigue and patient opt-outs require careful management to prevent automation from damaging rather than enhancing patient relationships. Establish frequency caps that prevent individual patients from receiving too many automated messages within specific timeframes, provide easy opt-out mechanisms for patients who prefer minimal communication while maintaining separate opt-in channels for critical appointment information, regularly audit automated sequences to eliminate redundancies or outdated content, and monitor opt-out rates as a key quality indicator, investigating spikes that suggest message frequency or relevance problems. Remember that automation should enhance communication quality, not just increase volume.
Measurement and attribution challenges make it difficult to prove automation ROI, particularly for metrics like patient lifetime value that unfold over extended periods. Combat this by establishing clear baselines before implementation, using control groups when possible to isolate automation effects from other practice changes, tracking leading indicators like engagement rates and response times that predict longer-term outcomes, and documenting anecdotal staff feedback and patient comments that qualitative benefits that numbers don't capture. Build a comprehensive ROI case that includes both quantitative metrics and qualitative improvements to maintain stakeholder support through inevitable implementation challenges.
Industry-Specific Best Practices for Dental Practice Automation
Dental practices have unique characteristics that require tailored automation approaches for optimal results. Understanding the dental patient journey—from awareness through treatment completion and ongoing maintenance—allows strategic placement of automated touchpoints at moments of maximum impact. Map automation to key decision points: initial inquiry responses that convert prospects to scheduled appointments, pre-visit sequences that reduce new patient no-shows, post-treatment follow-ups that ensure comfort and satisfaction, treatment plan education that overcomes cost and fear objections, and recall campaigns that maintain preventive care adherence. Each stage requires different messaging strategies, with awareness and consideration phases emphasizing education and trust-building while decision and action phases focus on convenience and value.
Leverage social proof and outcomes strategically throughout automated communications to address the fear and trust barriers unique to dental care. Approximately 50-60% of adults experience some dental anxiety, making credibility and reassurance critical elements of effective communication. Incorporate patient testimonials relevant to specific treatment types in educational sequences, highlight clinical outcomes and success rates for complex procedures, showcase team expertise and continuing education credentials, and include photos or videos of actual patients (with permission) rather than stock imagery. This social proof integration transforms automation from purely transactional communication into trust-building dialogue that accelerates patient progression through the care journey.
Establish a single source of truth dashboard that consolidates automation performance metrics with broader practice KPIs to enable data-driven decision making. Dental practices often struggle with fragmented data across practice management systems, automation platforms, websites, and marketing tools, making it difficult to understand true performance or identify improvement opportunities. Invest in dashboard development that integrates key metrics from all systems, providing unified visibility into patient acquisition costs, lifetime value, appointment show rates, treatment acceptance rates, and revenue cycle performance. Review this dashboard weekly in team huddles to celebrate wins, identify problems early, and maintain organizational focus on metrics that matter most.
Adopt a test-and-learn methodology that treats automation as an ongoing experiment rather than a set-it-and-forget-it solution. The most successful practices continuously test variations in message timing, content, delivery channels, and sequence structures, measuring results and scaling approaches that perform best. Start with small tests affecting limited patient segments before rolling successful approaches practice-wide, maintain a testing calendar that ensures continuous optimization without overwhelming staff, document learnings in a shared knowledge base so insights inform future decisions, and cultivate a culture where failed tests are viewed as valuable learning opportunities rather than mistakes. This iterative approach compounds improvements over time, with high-performing practices extracting 200-300% more value from automation investments compared to those who implement once and leave systems static.
Future-Proofing Your Dental Practice Automation Strategy
As automation technology continues evolving rapidly, practices must balance current implementation with strategic positioning for future capabilities. Artificial intelligence and machine learning will increasingly power dental practice automation, enabling conversational interfaces where patients interact with AI assistants for scheduling and basic questions, predictive models that optimize every aspect of practice operations, image analysis that automates aspects of diagnosis and treatment planning, and voice technology that allows hands-free interaction with practice systems during patient care. While cutting-edge AI capabilities may not be immediately accessible or affordable for all practices, selecting vendor partners with clear AI roadmaps positions practices to adopt innovations as they mature and become cost-effective.
Platform consolidation represents another significant trend, with comprehensive practice management systems increasingly incorporating automation capabilities that previously required separate point solutions. This consolidation simplifies technology stacks, reduces integration complexity, and often provides cost efficiencies compared to multiple standalone platforms. However, all-in-one platforms sometimes lag specialized solutions in specific capabilities. Evaluate whether consolidated platforms meet your specific automation requirements or if best-of-breed approaches with robust integration still provide superior results for your practice's unique needs and priorities.
Patient expectations around digital experience will continue rising, requiring practices to regularly refresh automation capabilities to meet evolving standards. What feels cutting-edge today becomes table stakes tomorrow as consumer technology giants train patients to expect frictionless digital interactions. Build technology refresh cycles into strategic planning, allocating budget for regular platform evaluations and upgrades, monitoring patient feedback about digital experience through surveys and reviews, studying automation implementations at leading practices to identify emerging best practices, and maintaining awareness of relevant innovations in adjacent industries like hospitality and retail that shape patient expectations. Practices that view automation as a strategic capability requiring ongoing investment rather than a one-time project will maintain competitive advantages as the industry continues evolving.
Frequently Asked Questions
Let’s level up your Dental Practices business
Need services that actually move the needle for Dental Practices? See our approach, pricing, and timelines—then book a quick call.
Additional Resources
- Schedule Your Dental Practice Automation Consultation
Book a complimentary 30-minute strategy session with our dental automation specialists. We'll review your current workflows, identify high-impact automation opportunities specific to your practice, discuss implementation timelines and investment requirements, and create a customized roadmap for transforming your practice operations while improving patient experience.
- View Our Dental Practice Automation Portfolio
Explore real-world case studies showcasing how we've helped dental practices implement automation systems that reduced administrative workload by 40-60%, improved appointment show rates by 15-25%, and increased treatment acceptance rates. See detailed before-and-after metrics, client testimonials, and specific automation workflows we've deployed across practices of all sizes.
- Free Dental Practice Automation Tools & Resources
Access our collection of free resources designed to help dental practices evaluate and implement automation successfully. Download automation ROI calculators, patient journey mapping templates, message template libraries, KPI tracking dashboards, vendor comparison guides, and implementation checklists. All resources are specifically tailored for dental practice operations and completely free to use.
Related Reading
Discover how automation for electricians streamlines scheduling, invoicing, lead tracking, and customer follow-ups to boost revenue and efficiency. Get started today.

Discover how automation streamlines furniture & home decor operations with GA4 tracking, attribution modeling, and data-driven dashboards. Get your 90-day implementation roadmap.
